Salmonella Dublin in dairy calves
MSU Extension provides an opportunity for people to understand this devastating disease of cattle.

The prevalence of Salmonella enterica subspecies enterica serovar Dublin (S. Dublin) infections in dairy cattle in the US has been increasing over the past years. The 2014 NAHMS study estimated S. Dublin to be present on 8% of dairy farms in the US, based on the presence of antibodies in one bulk milk sample. However, this likely is an underestimation of the real prevalence due to the limited sensitivity of the test used at that time, to detect the presence of the disease in a herd with just one bulk milk sample. In addition, several veterinary diagnostic laboratories had reported a progressive increase in the isolation of S. Dublin from diagnostic samples. Thus, suggesting that the prevalence of S. Dublin on dairy farms has increased in the last years.
The 2014 prevalence was higher in western dairy operations (52.1%) compared to midwestern dairy farms (4.4%). Nevertheless, at the US level, the proportion of affected operations were higher among larger herds (39.2% of herds milking over 500 cows) compared to smaller herds (1.0% of herds milking less than 100 cows, and 2.1% of herds milking 100 to 499 cows). Given the sustained increase in average farm size seen in the Michigan Dairy Industry in the past years, producers and veterinarians should be aware of the risks associated with the presence of S. Dublin in their herds. In fact, not only is S. Dublin the most commonly isolated serovar in clinical and nonclinical case submissions to the National Veterinary Services Laboratory, but also the number of S. Dublin isolates from samples submitted to the Veterinary Diagnostic Laboratory of Wisconsin State and Michigan State University has increased in the last decade. In the period between 2015 and 2019, S. Dublin represented 20.8% of all Salmonella spp. isolates in bovine samples at MSU’s diagnostic laboratory.
S. Dublin is the cattle host-adapted strain of Salmonella. Infection with S. Dublin can occur when susceptible calves ingest the bacteria shed by infected cows or calves. Diarrhea is a common consequence of Salmonella infections. However, the common presenting sign of S. Dublin infections is respiratory disease in calves 2 to 12 weeks of age. After colonizing the gastrointestinal tract, S. Dublin can spread through the bloodstream into organs such as the liver, spleen, or lymph nodes. Calves that survive the infection have a high probability of becoming in-apparent carriers for life.
Illness associated with S. Dublin can be difficult to treat and may be fatal. In addition to adult cattle and calves, people, other livestock and companion animal species are also susceptible to the infection. Carrier animals can maintain the infection within a herd and may continue to shed bacteria. A high proportion of the S. Dublin isolates from diagnostic samples at the MSU Veterinary Diagnostic Laboratory are resistant to most antimicrobials (Table 1). The purpose of this article is to highlight some of the key features of S. Dublin infections and management options available to control the disease.
DISEASE TRANSMISSION
S. Dublin is a host-adapted strain. Transmission usually occurs via the fecal-oral route. Although S. Dublin can cross the placenta, this likely leads to abortion rather than the birth of infected calves. The severity of the clinical presentation will vary with the infective dose (higher infective doses producing more severe clinical signs and more consistent shedding).
Once ingested, S. Dublin adheres and invades intestinal cells, crossing the small intestine, where it can be taken up by immune cells (macrophages) and transported to lymph nodes. Depending on the animals’ immunity, the immune system may be able to successfully kill the bacteria. Otherwise, the bacteria may be systematically distributed in lymph and blood, reaching to other organs like the lungs, liver, spleen, etc. causing septicemia.
S. Dublin can be shed not only in manure but also in the milk, saliva, urine, semen, and vaginal secretions of actively infected and carrier cattle. Hence, limiting the contact of susceptible animals with contaminated secretions is paramount to decrease the number of new infections. Therefore, hygiene and sanitation are key to reduce new infections.
CLINICAL SIGNS
Common Salmonella infections usually present as gastro-intestinal disease; however, S. Dublin most often presents as a respiratory illness. Calves less than six months old are at the highest risk for infection. Clinical signs observed in S. Dublin infected calves include:
- Hyperthermia (fever)
- Obtundation (depression)
- Anorexia (off-feed)
- Pneumonia
- Respiratory distress (e.g., elevated respiratory rate, coughing, etc.)
- Bloody diarrhea
- Dehydration
- Septicemia
Swollen joints, bone or brain infection are also possible following blood-borne spread of the bacteria. Clinical signs can also be chronic and include poor growth rates and ill-thrift.
DIAGNOSIS
There are two approaches to the diagnosis of S. Dublin. Testing may be used to detect the organism itself via fecal culture, or to detect the immune response of the animal via blood or milk ELISA. The organism can be detected by bacterial culture in a number of sample types. Fecal culture is the most common approach. However, shedding by infected carriers is intermittent and therefore negative results should be interpreted cautiously. Isolation from the more chronic clinical manifestations or from treated animals can be difficult. At postmortem examination, a wide range of tissues should be collected to increase the chance of successful isolation, for example, lung, liver, intestine, spleen, kidney and bone marrow.
The diagnostic sensitivity and specificity of the ELISA for antibody depends on the age of animal tested. The presence of maternally derived antibodies in calves less than 3 months of age complicates interpretation of the ELISA in this age group. Cross-reactions with other Salmonellae can occur. Hence, a positive serological finding should be followed up by attempts to culture the organism. Because of the time taken for an increase in the blood concentration of antibodies (i.e., seroconversion), serology is best used for retrospective diagnosis, or for monitoring purposes, and fecal culture for clinical diagnosis. Serological testing can also be carried out on milk samples. The monitoring of bulk milk antibody levels is used in the S. Dublin eradication schemes followed by some Scandinavian countries.
CONTROL OF Salmonella Dublin IN INFECTED HERDS
There are a number of measures that can be taken to address the spread of Salmonella Dublin in herds, either in the control of an outbreak, or to try to eradicate an endemic infection.
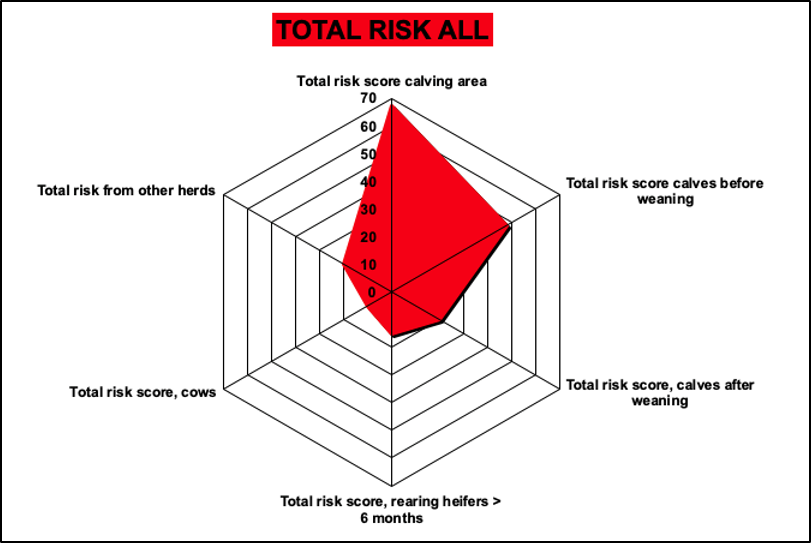
Management in many areas of a dairy farm are important in the control of S. Dublin infections. A risk assessment tool is available to identify areas of higher risk for the transmission of S. Dublin based on farm management practices (Figure 1). Dairy producers can contact MSU Extension to identify the major risk areas for S. Dublin transmission in their herds using this tool.
Calving area
The calving area represents one of the most critical areas to address in Salmonella control. Latent infections can reactivate around calving and active carriers shed in great numbers. Newborn calves are not able to fight infections at this time due to their underdeveloped immune system, making them very susceptible to infection. Hence, the calf with the dam allows transmission, and so calves should be removed as soon as possible within 2 hours after birth. Other cows, besides the calf’s own dam, present a risk through fecal shedding and cross-suckling. Reducing the number of cows present in the calving pen, replenishing bedding and disinfecting regularly, and avoiding using the calving pen as a hospital pen or grouping newborn calves (e.g., warming rooms, etc.) are important measures in reducing the spread of S. Dublin.
Calves younger than 3 months of age are most susceptible to infection with S. Dublin and general principles of good colostrum management apply, including avoiding pooling and maximizing cleanliness. Practices to minimize the contamination and growth of bacteria in the colostrum fed to calves are very important to avoid the infection of S. Dublin. Recommended colostrum storage practices are available here.
Pre-weaned calves
Maintaining an adequate plane of nutrition during this stage is critical for adequately supporting the calves’ immune system. However, feeding waste milk is a risk for exposure of calves to the bacterium, but pasteurization or acidification of the milk can be beneficial in this respect.
Maintaining a clean environment with appropriate stocking density will minimize exposure to fecal material. Sanitation is very important to minimize new infections in dairy calves. The contact of calves with adult cow feces should be avoided. Hence, sanitizing the feeding equipment is also very important to limit infections in newborn calves. Most classes of disinfectants used on dairy farms (e.g., aldehydes, alkalis, biguanides [chlorhexidine], halogens [sodium hypochlorite, iodine], quaternary ammonium compounds, etc.) are effective against gram-negative bacteria such as Salmonella. Removing organic material must always precede the use of any disinfectant. However, power washing of calf facilities is discouraged because it can aerosolize the bacteria thereby facilitating spread and contamination. Guidelines for cleaning and disinfection post confirmation of salmonellosis can be found here.
Heifer management
Similar principles apply to heifer management. The contact of heifers with older animals and their manure should be avoided. Mixing of groups should be kept at minimum and if managed on pasture, heifers should not be grazed on land previous spread with adult cow slurry. On stalls, hygiene of bedding and feed and water are important.
Mature cows
Appropriate stocking density and general hygiene are important in reducing the bacterial challenge to adult cattle. Cows are more susceptible to infection and more likely to become carriers if infected around the time of calving, likely due to decreased ability of the cows’ immune system to mount an effective response at this time. Therefore, attention to calving area management, reducing stress, and hygiene are crucial.
Identifying carrier animals is very challenging with the diagnostic tools available. Currently, the Animal Health Diagnostic Center at Cornell University categorizes a carrier as any animal that has 3 strong positive serum ELISA results over an 8-month period. Thus, requiring multiple testing to identify carrier animals. At the herd level, bulk tank samples can be used for periodic milking herd surveillance, or, if applied to selected milking groups, to identify whether S. Dublin has been introduced into a herd or is present in a particular population of cattle within the herd.
Biosecurity
Purchase of animals, particularly from multiple sources, is a significant risk factor for the introduction of S. Dublin into a herd. Given the intermittent shedding of carriers, quarantine screening using fecal testing has a low sensitivity. Clinically ill animals should be isolated from the herd and care should be taken not to return them too quickly to the main herd after the remission of clinical signs.
The bacterium can also be spread via inanimate objects (e.g., boots, clothes, equipment, etc.). Therefore, strong biosecurity practices with respect to visitors should be in place. S. Dublin can infect rodents and, therefore, control of rodents and protection of feed stores is important.
MANAGEMENT OF AN OUTBREAK
Dairy operations facing an increase in the number of cases of pneumonia, in many cases not responsive to antimicrobial treatment, should seek an investigation by their regular veterinarian. If S. Dublin is confirmed to be implicated in the outbreak, the producer should work with their veterinarian in establishing protocols to treat affected cattle and reduce new infections.
Treatment of Affected Calves
The treatment of calves infected by S. Dublin is directed to restore hydration status and correct electrolyte imbalances through fluid therapy, controlling inflammation with nonsteroidal anti-inflammatory drugs (NSAIDs) and treating bacteremia with antimicrobials in situations where a suitable drug is identified.
Administering an oral electrolyte solution between milk feedings will assist with the management of dehydration and acidosis. More severely affected calves would require intravenous fluid therapy with alkalinizing agents (e.g., bicarbonate) and energy sources like dextrose.
Calves suffering from nonspecific causes of diarrhea benefit from treatment with NSAIDs to control inflammation. Hence, their use is recommended despite no specific evidence for the treatment of S. Dublin. Available NSAIDs in the US include flunixin meglumine (injectable and transdermal) and meloxicam (oral). However, all NSAID use for treating diarrhea is extra-label and requires working with the farm’s veterinarian of record (the one maintaining a valid veterinarian-client-patient relationship) to determine the dose and frequency of administration, as well as the meat withholding time.
Appropriate antimicrobial selection is very challenging because most S. Dublin strains are multidrug resistant to antibiotics (Table 1). The isolated strains are not sensitive to any of the antimicrobials labeled for used in calves with septicemia. Thus, it is important to determine the susceptibility pattern of the strains affecting each herd to develop a therapeutic plan. In most cases, this would require the extra-label use of antimicrobials and the determination of meat withholding times as directed by the herd veterinarian.
| Year | ||
| Antimicrobial | 2018 (26 isolates) | 2019 (36 isolates) |
| Ampicillin | 0% | 0% |
| Ceftiofur | 4% | 6% |
| Clindamycin | 0% | 0% |
| Danofloxacin | 85% | 80% |
| Enrofloxacin | 65% | 83% |
| Florfenicol | 3% | 0% |
| Neomycin | 0% | 0% |
| Penicillin | 0% | 0% |
| Sulfadimethoxine | 4% | 0% |
| Trimethoprim/Sulfamethoxazole | 85% | 100% |
| Tetracycline | 0% | 0% |
| Tulathromycin | 62% | 88% |
The table above represents Antimicrobial susceptibility patterns of S. Dublin isolates (as % of susceptible isolates) at the MSU Veterinary Diagnostic Laboratory in the last two years.
However, some of the more effective antimicrobials are not allowed to use to treat this condition. For example, isolates of S. Dublin showed a similar pattern of high susceptibility to enrofloxacin in both the MSU diagnostic data (Table 1) and previous reports. Although the fluoroquinolone drug enrofloxacin is labelled for the treatment of bovine respiratory disease of non-lactating dairy cattle, the label is limited to disease associated with Mannheimia haemolytica, Pasteurella multocida, Histophilus somni and Mycoplasma bovis. Hence, using enrofloxacin to treat a S. Dublin infection would be considered extra-label usage, which is not allowed for fluoroquinolones in food-producing animal species. S. Dublin isolates also maintain high susceptibility patterns to potentiated sulfonamides (e.g., trimethoprim/sulfamethoxazole). Nevertheless, their use in pre-ruminant calves can lead to violative residues beyond the withdrawal time due to a slower elimination rate than adults. The withdrawal time should, therefore, be greatly extended compared with that for adult cattle.
Reduction of New Infections
Preventing the infection in new animals is another key element of the strategy to contain an outbreak. The factors mentioned before for the control in infected herds are of even greater importance when facing an outbreak. Particular emphasis should also be placed on sanitation practices and early identification and separation of calves showing signs of disease.
VACCINATION
Vaccination of cows and calves is another strategy that could contribute to preventing and controlling S. Dublin in dairy herds. However, published studies involving Salmonella vaccines on the market in the US have produced mixed results. Therefore, producers and veterinarians should carefully evaluate whether including these vaccines is warranted depending on each scenario. In a recent study, vaccination of dry cows with a S. Newport bacterin did not decrease mortality, clinical signs, sepsis, intestinal damage, or fecal shedding in neonatal calves infected with S. Typhimurium. Administration of a S. Dublin vaccine to dry cows to increase calf immunity against S. Dublin via colostrum can also be considered. Nevertheless, even though a study has proven that the administration of this vaccine to dry cows increases the transfer of specific passive immunity to the calf, whether these passively transferred antibodies offer protection against a Salmonella infection remains unexplored scientifically (although there are anecdotal reports of efficacy shutting down outbreaks from some veterinarians). Similarly, vaccination of newborn calves might prove useful in containing an outbreak. Another recent study has shown that oral or intranasal vaccination of calves at 4 and 18 days of age decreased mortality but did not improve the risk of pneumonia or weight gain. Also, the use of this vaccine in this fashion does not interfere with future diagnostic testing. Nevertheless, the use of the S. Dublin vaccine in calves is extralabel. Only veterinarians are allowed discretionary use of vaccines.
The authors thank Dr. Rinosh Mani from the MSU Veterinary Diagnostic Laboratory for providing the data relative to bovine samples tested for Salmonella Dublin.



 Print
Print Email
Email